COVID-19 and MS
Throughout this pandemic, MS Ireland have been carefully following developments regarding COVID-19 and MS. We have consulted with neurologists, our friends at MS Trust UK and other to ensure we are providing up-to-date, relevant and expert information. Below, is the information we have currently. This will be under continuous review as our knowledge expands and develops.
If you have specific concerns in relation to your own health or that of a loved one, we would advise that you contact your GP, MS nurse or neurologist.
NEW DIAGNOSIS
People experiencing symptoms suggestive of MS may experience delays in accessing neurology services due to the impact of COVID-19. Neurology centres have taken steps to mitigate potential issues and will, where possible, aim to carry out appropriate investigations in a timely manner in line with international guidelines.
If you are concerned about symptoms you have experienced and feel you may have MS, we advise that you make contact with your GP to discuss your concerns.
DISEASE MODIFYING THERAPIES DURING COVID-19
Those on disease-modifying therapies should remain on their treatments unless they are instructed by their neurologist to stop taking it. Further information can be found later in this document.
RELAPSE MANAGEMENT
Relapses should be reported to your neurology team who can provide advice.
A relapse involves the onset of a new symptom or worsening of symptoms for a period exceeding 24 hours in the absence of infection. Tiredness, heat, stress and infection can cause the temporary worsening of MS symptoms and this is not classed as a relapse.
Please see here for information on identifying a relapse can be found here
Information on the temporary worsening of symptoms can be found here
MONITORING
Safety monitoring should continue but the usual timings may be altered as a result of the COVID-19 pandemic. More information on monitoring can be found here
CLINIC APPOINTMENTS
Telemedicine may be utilised where appropriate. Information on preparing for your tele-medicine appointment can be found here
HOSPITAL DELIVERED THERAPIES
Measures will be taken to ensure that hospital delivered IV therapies will be carried out in a COVID-19 free ward with social distancing measures in place.
HOSPITAL APPOINTMENTS
If you have a hospital appointment and you have a cough, high temperature or shortness of breath, please do not come to the hospital, but contact your neurology team for advice.
GUIDANCE FROM THE NATIONAL CLINICAL PROGRAMME FOR NERUOLOGY IS AVAILABLE HERE
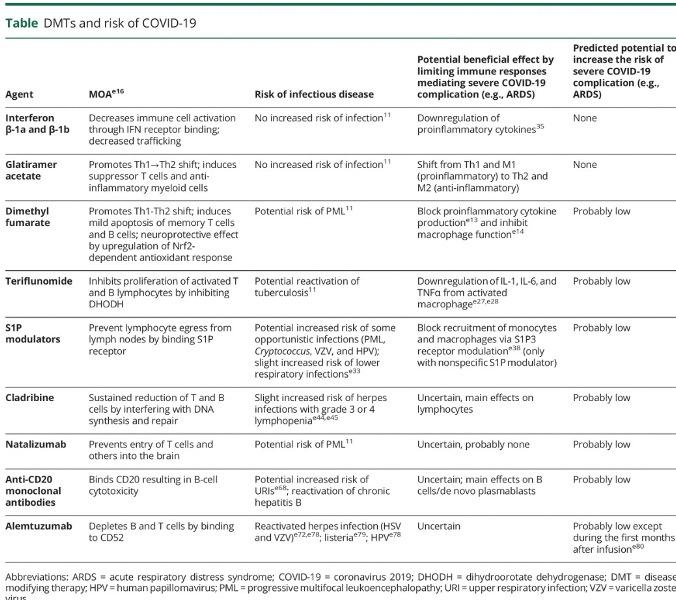
MS Medications during COVID-19
Some of the disease-modifying therapies used to treat MS work by suppressing the immune system. This can make a person more vulnerable to COVID-19. Please find information on the various medications below.
It is important not to stop MS treatments without instruction to do so by your neurologist as this can result in a rebound relapse in the following weeks or months, which can be severe. Individual treatment decisions should be discussed with your neurologist.
If you have a confirmed case of COVID-19 please contact your neurology team for advice on stopping your medicine.
Copaxone, Betaferon, Rebif, Avonex, Plegridy, Tecfidera and Aubagio
These medications should continue as normal. These medications are not believed to have much impact on how the immune system deals with COVID-19.
Tysabri
Tysabri is not believed to effect the way the immune system deals with COVID-19. Those receiving Tysabri should continue to receive it. When starting Tysabri the first 3 infusions should be administered monthly. After this, the infusion may be given every 6 weeks, this may give further protection from viruses that can enter the nervous system but not affect Tysabri's effectiveness, with appropriate monitoring. Please do not stop Tysabri abruptly as this could cause rebound in MS inflammation after a few months.
Gilenya
Gilenya may have some issues with COVID-19 but there is no detailed information currently available. If you are taking this medication you should continue with it unless you are instructed by a healthcare professional to stop. Stopping this medication suddenly may increase the risk of a rebound relapse in the following weeks and months.
Ocrevus, Lemtrada, Rituximab and Mavenclad
These treatments may make a person more vulnerable to COVID-19. You may be asked to delay your treatment, but this decision is made by the neurologist on a case by case basis. These medications often have a prolonged therapeutic effect and so delaying planned infusions or starting one of these drugs is not a major problem.
It is currently considered safe to start or receive retreatment of Mavenclad or Ocrevus and to continue treatment with Lemtrada and Rituximab, for those who meet the clinical indication of these therapies.
Mayzent (Siponimod) and Arezza (Ofatumumab)_
These medications are not easily available in Ireland. If you have specific queries please contact your neurologist.
Autologous Haematopoietic Stem Cell Transplant (HSCT)
Treatment may be delayed for a number of months. Further discussion with your neurologist is important in relation to this. If you have any queries, please contact a healthcare professional for more detailed advice.
Steroids for MS relapses
The type of steroids used in MS relapses management can interfere with the bodies response to viral infections. Generally, for people who have active COVID-19, the use of steroids to treat a relapse would be avoided if possible but if the relapse is severe then the benefits of using steroids may outweigh the risks. This decision would need to be made on an individual basis. If you have active COVID-19 and experience a relapse, we advise that you make contact with your neurology team for individual advice.
It is worth noting that steroids may aid the speed of relapse recovery but not the extent of the recovery.
For those who do not have COVID-19, steroids can be given if clinically required. These people would be advised to cocoon for two weeks after a course of steroids to reduce the risk of contracting COVID-19
If you have any concerns, please contact a healthcare professional for more detailed advice.
Hospital appointments:
If you have an appointment to come to hospital for a review or treatment, and you have cough, high temperature or shortness of breath please do not come to the hospital, but contact your MS team for advice
Symptoms of COVID-19
The symptoms of COVID-19 are:
- a cough
- shortness of breath
- breathing difficulties
- fever (high temperature)
- Chills
It can take up to 14 days for symptoms of coronavirus to appear.
Hygiene and prevention
The most important action we can all take to help prevent the spread of Covid-19 is good hand and respiratory hygiene.
MS Ireland encourages everyone to read the HSE’s Coronavirus Information page -https://www2.hse.ie/conditions/coronavirus/protect-yourself.html including the do’s and don’ts:
Do:
- Wash your hands properly and regulary.
- Cover your mouth and nose with a tissue or your sleeve when you cough or sneeze.
- Put used tissues into a bin and wash your hands.
- Clean and disinfect frequenty touched objects (such as phones, remote controls etc,) and surfaces.
Don’t
- Do not touch your eyes, nose or mouth if your hands are not clean.
Handwashing
The HSE has also issued the following essential advice on when precisely to wash your hands:
- After coughing or sneezing.
- After toilet use.
- Before eating.
- Before and after preparing food.
- If you are in contact with a sick person, especially those with respiratory symptoms.
- If your hands are dirty.
- If you have handled animals or animal waste.
Step-by-step guide on how to properly wash your hands and avoid infection:
- Wet your hands with warm water and apply soap.
- Rub your hands together until the soap forms a lather.
- Rub the top of your hands, between your fingers and under your fingernails.
- Do this for at least 20 seconds.
- Rinse your hands under running water.
- Dry your hands with a clean towel or paper towel.

TEMPORARY WORSENING OF SYMPTOMS AND COVID-19
It is an important time to note that a number of factors can result in the reappearance or worsening of MS symptoms (sometimes referred to as a pseudo-relapse).
If you have been in contact with a confirmed case
If you are displaying symptoms of COVID-19
If you develop symptoms of COVID-19 , avoid contact with people by self-isolating (see below) and phone your GP.
Do not go to your GP’s practice, pharmacy or hospital. Your GP will assess you over the phone. If you do not have a GP, phone 112 or 999.
Your GP will arrange a test and can organize for the National Ambulance Service or other emergency services to deliver the test. If you do not drive please inform your GP.
Advice on self-isolating
Advice on self-isolating
Self-isolation means staying indoors and avoiding contact with other people. If there is a chance you could have coronavirus, you may be asked to stay away from other people (self-isolate). This will help to prevent the spread of coronavirus to others.
Information from the HSE on how to self-isolate can be found here:
If you have a confirmed case of COVID-19
If you have a confirmed case of COVID-19 please contact your neurology team for further detailed advice.
MS Ireland Regional Contact
MS Ireland have altered the way in which we work with our members, in line with Government guidance. The safety of the MS community and our staff is of paramount importance and so precautionary measures have been be put in place to prevent the spread of COVID-19. While face-to-face visits may not be possible, our staff are contactable via telephone. Regional contact information can be found here.
Useful links:
HSE up-to-date advice on corona virus:
World Health Organisation (WHO): Advice to the public
Multiple Sclerosis International Federation (MSIF) – Coronavirus and MS: What You Need to Know
Department of Foreign Affairs up-to-date travel advice
Association of British Neurologists Guidance on MS DMT’S and Coronavirus